Empowerment Through Knowledge: Conquering Low Back Pain
Low back pain is a common and often debilitating condition that can affect people of all ages and backgrounds. Whether it’s a dull, nagging ache or a sharp, intense pain, low back pain can significantly impact your quality of life. In this blog post, we will explore the various aspects of low back pain, from its causes and symptoms to prevention and treatment options. Whether you’re currently suffering from low back pain or simply interested in learning more about it, this comprehensive guide aims to provide you with the knowledge and insights you need.
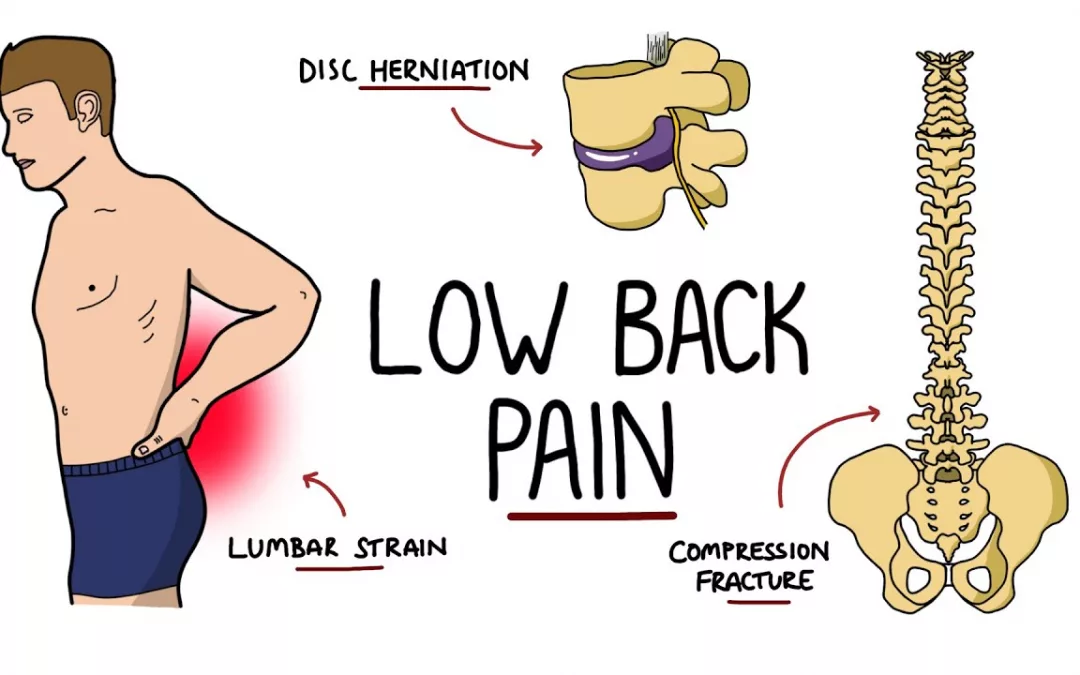
What is Low Back Pain?

Low back pain, often abbreviated as LBP, refers to discomfort, pain, or soreness in the lower part of the back, specifically the lumbar region. It is one of the most prevalent musculoskeletal disorders globally, affecting people of all ages. Low back pain can be acute (short-term) or chronic (long-lasting), and its severity can range from mild to severe.
Types of Low Back Pain

Low back pain can manifest in various forms and be categorized based on its characteristics and underlying causes. Understanding the types of low back pain is essential for accurate diagnosis and effective treatment. Here are some common types:
- Mechanical Low Back Pain:
- Acute Mechanical Low Back Pain: This type of pain is typically caused by sudden trauma or strain, such as lifting a heavy object improperly or overexertion during physical activity. It is usually short-lived and may resolve with rest and self-care.
- Chronic Mechanical Low Back Pain: Chronic mechanical low back pain results from ongoing wear and tear on the spine or muscles. It can be associated with muscle imbalances, poor posture, or repeated microtrauma. This type of pain lasts for 12 weeks or longer.
- Radicular Pain (Sciatica): Radicular pain occurs when a spinal nerve root is compressed, leading to pain that radiates along the nerve’s path. Sciatica is a common form of radicular pain, characterized by sharp, shooting pain that travels down one leg. It is often caused by a herniated disc or spinal stenosis.
- Referred Pain: Referred pain is discomfort that is felt in the lower back but originates from a different location, such as the internal organs. For example, kidney stones or infections may cause referred pain in the lower back.
- Degenerative Disc Disease: This condition is not a disease but rather a natural part of aging. Over time, the intervertebral discs that cushion the spine can lose their elasticity and become less effective at absorbing shock. This can lead to chronic, dull low back pain.
- Spinal Stenosis: Spinal stenosis is a condition characterized by the narrowing of the spinal canal. This can put pressure on the spinal cord and nerves, causing pain, numbness, and weakness in the lower back and legs. Spinal stenosis may be caused by age-related changes in the spine or by structural abnormalities.
- Ankylosing Spondylitis: Ankylosing spondylitis is a form of inflammatory arthritis that primarily affects the spine, causing stiffness and pain. It typically begins in the sacroiliac joints (located at the base of the spine) and can lead to chronic low back pain.
- Fibromyalgia: Fibromyalgia is a chronic condition characterized by widespread pain and tenderness in the muscles, ligaments, and tendons. Low back pain is a common symptom for individuals with fibromyalgia.
- Spondylolisthesis: This condition occurs when one vertebra slips forward over the one below it. It can cause lower back pain and may also lead to nerve compression.
- Piriformis Syndrome: The piriformis is a small muscle in the buttocks. When it becomes tight or spasms, it can compress the sciatic nerve and result in symptoms similar to sciatica.
- Muscle Imbalance or Weakness: Imbalances in the muscles supporting the spine, including the core muscles, can lead to low back pain. These imbalances can result from poor posture, sedentary lifestyles, or previous injuries.
It’s important to note that an individual may experience a combination of these types of low back pain, and the specific diagnosis can vary from person to person. Accurate diagnosis by a healthcare professional is critical to tailor treatment and management strategies effectively. The treatment approach for low back pain depends on its cause and may include physical therapy, medication, exercise, and, in some cases, surgery.
Causes of Low Back Pain

Low back pain can have a wide range of causes, and identifying the specific underlying factor is crucial for effective treatment and management. Here are some common causes of low back pain:
- Muscle Strain or Sprain:
- Cause: Overexertion, poor posture, lifting heavy objects, or sudden movements can strain the muscles and ligaments in the lower back.
- Symptoms: Dull, aching pain in the lower back, muscle stiffness, and limited range of motion.
- Herniated Disc (Bulging or Slipped Disc):
- Cause: When the soft inner core of an intervertebral disc protrudes through its tough outer layer, it can compress nearby nerves and cause pain.
- Symptoms: Sharp, shooting pain in the lower back that may radiate into the buttocks or legs, numbness or tingling.
- Sciatica:
- Cause: Compression or irritation of the sciatic nerve, which runs from the lower back down the legs, can result in radiating pain, often referred to as sciatica.
- Symptoms: Shooting pain, burning sensation, or electric shock-like pain that travels down one or both legs, weakness or numbness.
- Spinal Stenosis:
- Cause: Spinal stenosis involves the narrowing of the spinal canal, which can put pressure on the spinal cord and nerves.
- Symptoms: Pain, numbness, or weakness in the lower back and legs, usually worsened by walking or standing.
- Arthritis:
- Cause: Conditions like osteoarthritis, rheumatoid arthritis, and ankylosing spondylitis can lead to inflammation and joint pain in the lower back.
- Symptoms: Stiffness, pain, and reduced range of motion in the lower back, often worse in the morning.
- Spondylolisthesis:
- Cause: Spondylolisthesis occurs when one vertebra slips forward over the one below it, leading to lower back pain and, in some cases, nerve compression.
- Symptoms: Lower back pain, muscle tightness, and radiating pain if nerves are affected.
- Piriformis Syndrome:
- Cause: The piriformis is a small muscle in the buttocks. When it tightens or spasms, it can compress the sciatic nerve and cause symptoms similar to sciatica.
- Symptoms: Pain in the buttocks that may radiate down one leg, often mistaken for sciatica.
- Kidney Stones or Infections:
- Cause: Problems with the kidneys, such as kidney stones or infections, can cause referred pain in the lower back.
- Symptoms: Low back pain, often accompanied by urinary symptoms, such as frequent urination or blood in the urine.
- Degenerative Disc Disease:
- Cause: This condition is not a disease but rather a natural part of aging. Over time, the intervertebral discs that cushion the spine can lose their elasticity and become less effective at absorbing shock.
- Symptoms: Chronic, dull low back pain that worsens with movement.
- Fibromyalgia:
- Cause: Fibromyalgia is a chronic condition characterized by widespread pain and tenderness in the muscles, ligaments, and tendons.
- Symptoms: Low back pain is one of many symptoms, along with fatigue, sleep disturbances, and cognitive issues.
It’s important to note that low back pain can result from a combination of factors, and the specific cause may vary from person to person. Accurate diagnosis by a healthcare professional is critical to tailor treatment and management strategies effectively. The choice of treatment depends on the underlying cause and may involve a combination of self-care, physical therapy, medication, and, in some cases, surgery.
Symptoms of Low Back Pain

Low back pain can present with a variety of symptoms, and the specific manifestations may vary depending on the underlying cause and individual factors. Here are some common symptoms associated with low back pain:
- Dull or Aching Pain: Many individuals with low back pain experience a persistent, dull, or aching discomfort in the lower back region. This pain can range from mild to severe and may be constant or intermittent.
- Radiating Pain (Sciatica): Sciatica is a common symptom of low back pain that occurs when the sciatic nerve, which runs from the lower back down the legs, is compressed or irritated. This can result in sharp, shooting pain that radiates down one or both legs.
- Muscle Spasms: Low back pain often leads to muscle spasms or cramping in the lower back. These spasms can contribute to additional discomfort and stiffness.
- Reduced Flexibility: Low back pain can limit a person’s range of motion, making it difficult to bend, twist, or move freely. This reduced flexibility can be especially noticeable when attempting activities that involve the lower back.
- Difficulty Standing Up Straight: Some individuals with low back pain may find it challenging to maintain an upright posture, causing them to hunch forward or lean to one side.
- Numbness or Tingling: When low back pain is associated with nerve compression, such as in cases of herniated discs or spinal stenosis, numbness or tingling sensations may occur in the lower back, buttocks, or legs.
- Weakness: Muscular weakness, particularly in the legs, can be a symptom of low back pain, especially if it’s related to nerve compression. Weakness may affect mobility and coordination.
- Pain Aggravated by Certain Activities: Low back pain may worsen with specific activities, such as lifting heavy objects, prolonged sitting or standing, bending, or twisting. The pain may be more noticeable during or after these activities.
- Pain Relief with Rest: In cases of acute low back pain, rest and a change in activity may provide relief. Individuals with muscle strains or minor injuries may find that pain subsides with rest.
- Chronic Pain: Chronic low back pain, which persists for 12 weeks or longer, is often characterized by ongoing discomfort. This pain can be relatively consistent or may have periods of exacerbation and improvement.
- Painful Mornings: Some individuals with low back pain report increased discomfort in the morning, which may improve as they become more active throughout the day.
- Pain During Certain Movements: Low back pain can be triggered or exacerbated by specific movements, such as bending forward, lifting, or twisting. These movements may place added stress on the lower back.
It’s important to note that low back pain is a complex condition, and individuals may experience a combination of these symptoms. Accurate diagnosis by a healthcare professional is essential to determine the underlying cause of the pain and develop an appropriate treatment plan.
Diagnosing Low Back Pain

Diagnosing the cause of low back pain is a crucial step in developing an effective treatment plan. Healthcare professionals use a combination of methods and assessments to identify the underlying cause of low back pain. Here’s an overview of the diagnostic process:
- Medical History:
- The healthcare provider will begin by taking a detailed medical history. This involves asking the patient about the onset of pain, its duration, and any specific events or activities that might have triggered the pain. They will also inquire about the character and location of the pain, as well as any other symptoms, such as numbness, tingling, or weakness.
- Physical Examination:
- A physical examination is performed to assess the patient’s posture, range of motion, and areas of tenderness in the lower back. The healthcare provider will look for signs of inflammation, muscle tightness, or any physical abnormalities that may contribute to the pain.
- Neurological Examination:
- To assess nerve function and identify any neurological issues, the healthcare provider may conduct a neurological examination. This can include testing reflexes, muscle strength, and the sensation in various areas of the lower back and legs.
- Imaging Studies:
- Imaging studies are often necessary to visualize the structures of the spine and identify any structural abnormalities. Common imaging modalities include:
- X-rays: X-rays can provide detailed images of the bones and help identify issues like fractures, bone spurs, or changes in spinal alignment.
- Magnetic Resonance Imaging (MRI): An MRI can show the soft tissues of the spine, including discs, nerves, and ligaments. It is useful for identifying issues like herniated discs or spinal stenosis.
- Computed Tomography (CT) Scan: CT scans can provide detailed images of the bones and can be especially helpful in identifying fractures and bone abnormalities.
- Bone Scans: In cases where bone abnormalities are suspected, a bone scan may be used to detect areas of increased bone activity.
- Imaging studies are often necessary to visualize the structures of the spine and identify any structural abnormalities. Common imaging modalities include:
- Laboratory Tests:
- Blood tests are not typically used to diagnose low back pain, but they can be ordered to rule out certain underlying conditions, such as infections or inflammatory disorders.
- Specialized Tests:
- In some cases, specialized tests or diagnostic procedures may be needed, especially if the cause of low back pain remains unclear. These may include:
- Electromyography (EMG): An EMG measures the electrical activity of muscles and nerves and can help identify nerve-related issues.
- Discography: A discography involves injecting a contrast dye into the intervertebral discs to identify the source of disc-related pain.
- Nerve Blocks: Nerve blocks involve injecting anesthetic or anti-inflammatory medications into specific nerves to determine if they are the source of pain.
- In some cases, specialized tests or diagnostic procedures may be needed, especially if the cause of low back pain remains unclear. These may include:
- Consultation with Specialists:
- Depending on the initial assessments and test results, the healthcare provider may refer the patient to specialists such as orthopedic surgeons, neurologists, or pain management experts for further evaluation and guidance.
Once a clear diagnosis has been established, the healthcare provider can develop a treatment plan tailored to the specific cause of the low back pain. Treatment options may include medication, physical therapy, exercise, lifestyle modifications, and, in some cases, surgical interventions. The goal is to relieve pain, improve function, and address the underlying issue to prevent future recurrences of low back pain.
Treatment Options for Low Back Pain

The treatment for low back pain depends on its underlying cause, the severity of symptoms, and the individual’s overall health. Treatment options can vary widely, and a healthcare provider will determine the most appropriate approach for each specific case. Here are some common treatment options for low back pain:
- Rest and Activity Modification:
- In cases of acute low back pain, short-term rest may be recommended to allow the injured tissues to heal. It’s essential to balance rest with periods of gentle activity to prevent muscle stiffness.
- Medications:
- Medications are often used to manage pain and reduce inflammation associated with low back pain. Common medications include:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These over-the-counter or prescription drugs help reduce pain and inflammation, including ibuprofen, naproxen, and prescription-strength NSAIDs.
- Muscle Relaxants: These medications can alleviate muscle spasms and tension in the lower back.
- Pain Relievers: Over-the-counter pain relievers, such as acetaminophen, can help manage pain. In some cases, prescription pain medications may be necessary for severe pain.
- Medications are often used to manage pain and reduce inflammation associated with low back pain. Common medications include:
- Physical Therapy:
- Physical therapists can design customized exercise and stretching programs to strengthen the muscles of the lower back, improve flexibility, and correct posture. Physical therapy aims to reduce pain and prevent recurrences.
- Heat and Cold Therapy:
- Applying heat or cold to the affected area can help relieve muscle spasms and reduce inflammation. Cold packs are typically used in the acute phase of pain, while heat therapy is more appropriate for chronic conditions.
- Chiropractic Care or Osteopathic Manipulation:
- Chiropractors and osteopathic physicians can perform spinal adjustments and manipulations to improve spinal alignment and alleviate pain.
- Acupuncture:
- Some individuals find relief from low back pain through acupuncture, a complementary therapy that involves inserting thin needles into specific points on the body.
- Ergonomic Changes:
- Modifying the workspace or home environment can help reduce strain on the lower back. Using chairs with proper lumbar support, maintaining good posture, and using ergonomic office equipment can make a significant difference.
- Lifestyle Modifications:
- Lifestyle changes, such as maintaining a healthy weight, staying physically active, and managing stress, are important for preventing and managing low back pain.
- Education:
- Learning about the condition can empower individuals to make informed decisions about their care. It’s essential to understand proper body mechanics and ergonomic principles.
- Nerve Blocks or Epidural Injections:
- In cases of severe pain or nerve compression, nerve blocks or epidural injections of corticosteroids may be recommended to provide temporary relief.
- Pain Management Programs:
- Comprehensive pain management programs may be beneficial for individuals with chronic low back pain. These programs often include a combination of therapies, education, and psychological support.
- Surgical Interventions:
- Surgery is generally considered when conservative treatments have not provided relief or when there’s a specific structural issue requiring intervention. Common surgical procedures for low back pain include discectomy (removing part of a herniated disc), spinal fusion, and laminectomy (removing a portion of a vertebra).
The choice of treatment depends on the individual’s diagnosis, overall health, and the severity of their low back pain. Healthcare providers will work closely with patients to develop a tailored treatment plan with the goal of alleviating pain, improving function, and preventing future recurrences of low back pain.
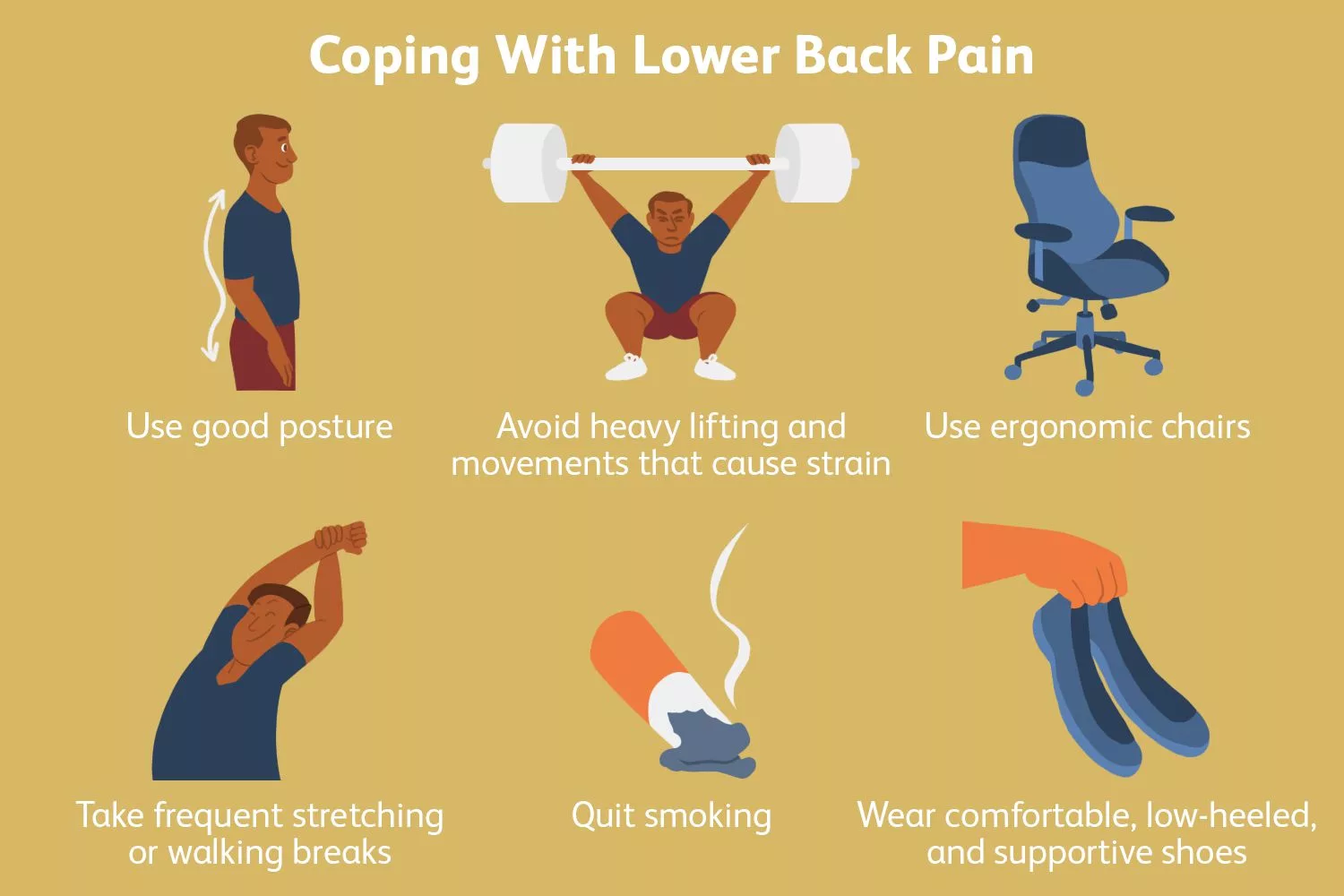
Preventing Low Back Pain

Preventing low back pain is essential for maintaining good spinal health and overall well-being. While it may not be possible to completely eliminate the risk, adopting healthy lifestyle habits and ergonomic practices can significantly reduce the likelihood of experiencing low back pain. Here are some strategies for preventing low back pain:
- Maintain a Healthy Weight:
- Excess body weight can place additional stress on the lower back. Maintaining a healthy weight through a balanced diet and regular exercise can reduce the risk of low back pain.
- Regular Physical Activity:
- Engage in regular exercise to strengthen the muscles that support the lower back. Activities like walking, swimming, and yoga can help improve flexibility and reduce the risk of injury.
- Proper Lifting Techniques:
- When lifting objects, use your legs to lift rather than your back. Bend your knees, keep the object close to your body, and avoid twisting while lifting.
- Maintain Good Posture:
- Practice good posture while sitting, standing, and walking. Use ergonomic chairs and workstations to support proper posture while working at a desk.
- Stretch and Strengthen:
- Incorporate stretching and strengthening exercises for the back, core, and leg muscles into your fitness routine. This can help improve flexibility and stability.
- Stay Active:
- Avoid prolonged periods of inactivity, whether sitting or standing. Take short breaks to change your position and stretch periodically.
- Ergonomic Workspaces:
- Adjust your workspace to minimize strain on the lower back. Use chairs with lumbar support, position your computer monitor at eye level, and maintain an ergonomic setup.
- Proper Footwear:
- Choose comfortable and supportive shoes that provide adequate arch support. Good footwear can help maintain proper alignment from the ground up.
- Use Safe Lifting Equipment:
- When lifting heavy objects, consider using equipment like lifting belts or carts to reduce the risk of injury.
- Quit Smoking:
- Smoking can reduce blood flow to the spine and inhibit the body’s ability to heal, making smokers more susceptible to low back pain.
- Manage Stress:
- Chronic stress can lead to muscle tension and pain. Engage in stress-reduction techniques like meditation, deep breathing exercises, or mindfulness to promote relaxation.
- Sleep Position:
- Pay attention to your sleeping posture. Use a mattress and pillow that provide adequate support for your spine. Sleeping on your side with a pillow between your knees can help maintain proper alignment.
- Hydrate and Maintain a Balanced Diet:
- Staying hydrated is crucial for the health of your spinal discs. A balanced diet rich in nutrients can promote overall musculoskeletal health.
- Stay Hydrated:
- Proper hydration is important for the health of spinal discs. Drink an adequate amount of water daily to support disc function.
- Know Your Limitations:
- Be aware of your physical limitations and avoid overexerting yourself. Listen to your body and don’t push beyond your capabilities.
It’s important to remember that low back pain can result from various factors, and no single prevention strategy can guarantee avoidance of the condition. However, by adopting a combination of these preventive measures, you can significantly reduce the risk and promote better spinal health. If you experience persistent or severe low back pain, seek medical evaluation and guidance for appropriate diagnosis and treatment.
Living with Chronic Low Back Pain
Living with chronic low back pain can be challenging, but with the right strategies and support, it is possible to manage the condition and maintain a good quality of life. Chronic low back pain is typically defined as pain that lasts for 12 weeks or longer. Here are some tips for living with chronic low back pain:
- Medical Management:
- Consult with a healthcare provider or pain specialist to develop a tailored treatment plan. This may include medications, physical therapy, or other interventions to manage pain and improve function.
- Pain Management Techniques:
- Learn and practice pain management techniques such as relaxation, deep breathing exercises, or meditation to reduce the impact of pain on your daily life.
- Physical Activity:
- Stay active within the limits of your pain. Engage in exercises that are gentle on the back, such as walking or swimming. Physical activity can help maintain strength and flexibility.
- Physical Therapy:
- Work with a physical therapist to develop a customized exercise program that targets core strength, flexibility, and posture. These exercises can help stabilize the spine and reduce pain.
- Ergonomic Support:
- Make ergonomic changes in your home and workspace to reduce strain on your back. This may include using supportive chairs, maintaining proper posture, and adjusting your computer setup.
- Weight Management:
- Maintain a healthy weight to reduce the strain on your lower back. Weight loss can help alleviate pain and reduce the risk of exacerbating the condition.
- Supportive Footwear:
- Choose comfortable and supportive shoes that provide proper arch support. Good footwear can have a positive impact on overall posture and spinal health.
- Pain Medications:
- Follow your healthcare provider’s recommendations regarding pain medications. These may include nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, or, in some cases, opioids.
- Heat and Cold Therapy:
- Use heat or cold therapy as directed to relieve muscle spasms and reduce inflammation. Experiment with different methods to determine which provides the most relief.
- Psychological Support:
- Chronic pain can take a toll on mental health. Seek support from a mental health professional to address the emotional aspects of living with pain, such as anxiety or depression.
- Stress Management:
- Engage in stress-reduction techniques like meditation, mindfulness, or yoga to reduce the emotional impact of chronic pain.
- Sleep Hygiene:
- Pay attention to your sleep habits. Ensure that your mattress and pillow provide adequate support and practice good sleep hygiene to improve the quality of your rest.
- Supportive Network:
- Connect with friends and family who understand your condition and can provide emotional support. Support groups or online communities for people with chronic pain can also be valuable.
- Pacing and Energy Conservation:
- Recognize your limitations and avoid overexertion. Break tasks into smaller, manageable segments, and take breaks as needed to conserve energy.
- Set Realistic Goals:
- Focus on setting achievable goals and milestones to avoid frustration. Gradual progress is more sustainable than attempting significant changes all at once.
Remember that chronic low back pain is a complex condition, and it may take time to find the right combination of treatments and strategies that work for you. Be patient with yourself and work closely with healthcare professionals to manage your pain and improve your quality of life.
Conclusion: Low Back Pain

Low back pain is a complex and widespread issue that affects millions of people around the world. By understanding its causes, symptoms, diagnosis, treatment options, prevention strategies, and the challenges of living with chronic low back pain, individuals can make informed decisions about their care and take steps to prevent or effectively manage this condition. By taking proactive measures and seeking appropriate treatment, you can improve your quality of life and alleviate the burden of low back pain. Whether you’re someone who has experienced low back pain or you’re seeking information to support a loved one, this comprehensive blog post provides valuable insights into this common and often debilitating condition.
BEST CHIROPRACTOR NEAR ME IN ORLANDO, FLORIDA
CALL NOW +1-407-434-7246
If you have suffered any type of injury or have been experiencing pain that just won’t go away regardless of what you do, then all you have to do is call and speak with our friendly staff. Find Best Chiropractic Care in Orlando, Florida. Our team can help you get the treatment you need and ensure that the pain you experience is alleviated – once and for all.
We are proud to serve the areas of Orlando, Altamonte Springs, Haines City, Plant City, Kissimmee, Winter Haven, and Ocala.
Contact us for Chiropractor near me in Orlando, Florida for an Appointment Today.
How do I know if my lower back pain is serious?
Back pain accompanied by sensations of numbness, tingling or weakness could be a sign of nerve irritation or damage. This is especially true if the pain persists after taking over-the-counter (OTC) pain relievers. Nerve pain is serious and can result in permanent damage or disability if left untreated.
How do you relieve low back pain?
Gentle exercise, such as walking, swimming, yoga, cycling or simple stretching, increases blood flow and promotes healing. Also, strengthening your core (abdominal and back muscles) can help relieve back pain. Without any movement, the muscles around your spine may feel stiff or weak, making low back pain even worse.
How can I tell if my back pain is kidney related?
Back problems usually affect your lower back. Kidney pain is felt higher and deeper in your body than back pain. You may feel it in the upper half of your back, not the lower part. Unlike back discomfort, it's felt on one or both sides, usually under your rib cage.
What causes lower back pain just above the buttocks?
While lower back pain just above the buttocks can be a hassle to deal with, something as simple as a muscle strain or common conditions like sciatica or muscle spasms can cause it. Less vigorous activity and basic home care can reduce the pain from these conditions.
What is the average age for lower back pain?
As you age, your spine goes through changes that make it more delicate and susceptible to pain. For most people, the first back pain symptoms arise between age 30 and 50, and they keep getting worse from there on out. Most of the time, age-related back pain can be attributed to general degeneration.