Understanding the Basics of a Herniated Disc
What is a herniated disc? Herniated disc often referred to as slipped disc or ruptured disc is a common and often painful spinal condition that affects millions of people worldwide. Whether you’re experiencing back pain yourself or simply curious about this condition, this comprehensive blog post will provide you with an in-depth understanding of what a herniated disc is, its causes, symptoms, available treatment options, and what you can expect during the recovery process.
Anatomy of a Herniated Disc
Before we delve into the intricacies of herniated discs, it’s essential to have a basic understanding of the spine’s anatomy. The spine, also known as the vertebral column, is a complex structure made up of 33 individual vertebrae, divided into five regions:
- Cervical spine: Comprising seven vertebrae (C1-C7), the cervical spine is located in the neck.
- Thoracic spine: The middle section of the spine, consisting of twelve vertebrae (T1-T12).
- Lumbar spine: Located in the lower back, the lumbar spine is made up of five vertebrae (L1-L5).
- Sacral spine: These vertebrae are fused together to form the sacrum, a triangular bone at the base of the spine.
- Coccygeal spine: The coccyx, also known as the tailbone, is made up of fused coccygeal vertebrae at the very bottom of the spine.
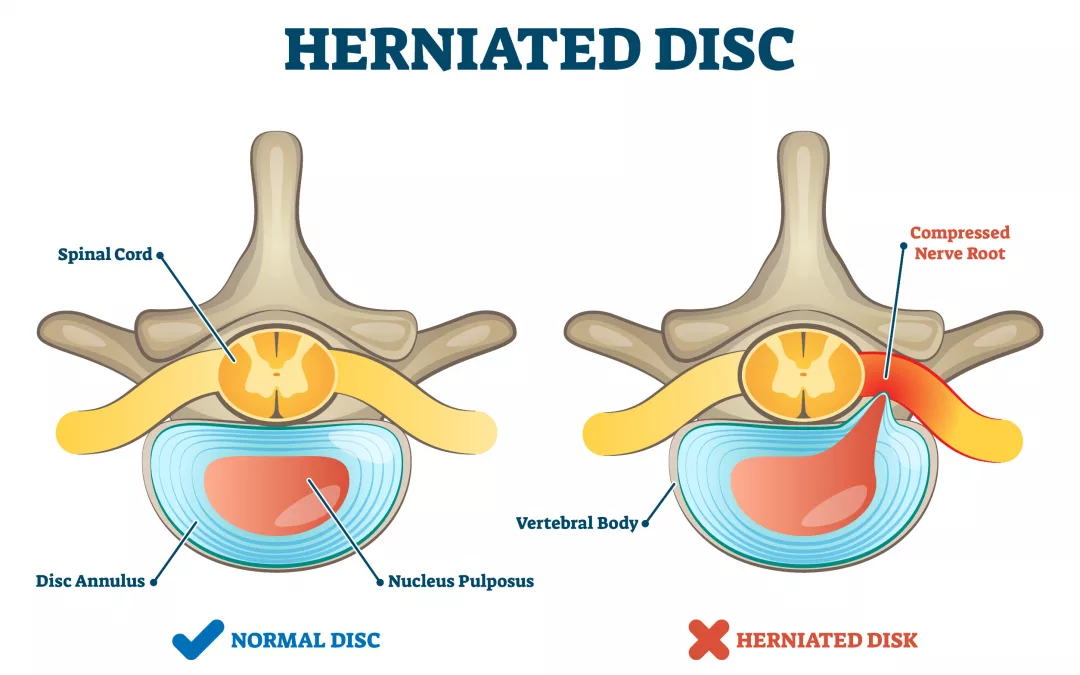
Between each pair of adjacent vertebrae, there are intervertebral discs that serve as cushions, allowing for flexibility and shock absorption in the spine. These discs have two main components:
- Annulus fibrosus: The tough outer ring of fibrous tissue that encases the disc’s inner core.
- Nucleus pulposus: The soft, jelly-like inner core.
A herniated disc occurs when the inner core (nucleus pulposus) pushes through or ruptures the outer ring (annulus fibrosus) of the disc. This condition is also known as a disc protrusion or disc herniation.
Causes of Herniated Disc
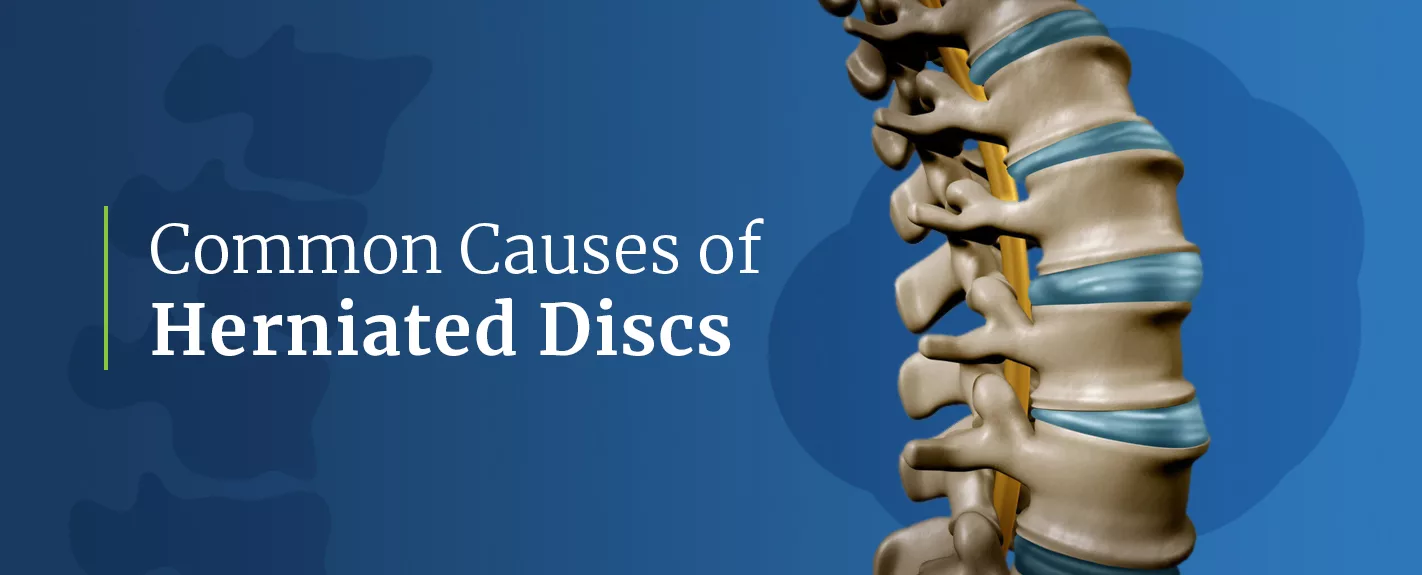
Understanding the underlying causes of herniated disc is crucial for both prevention and management. Several factors contribute to the development of herniated discs:
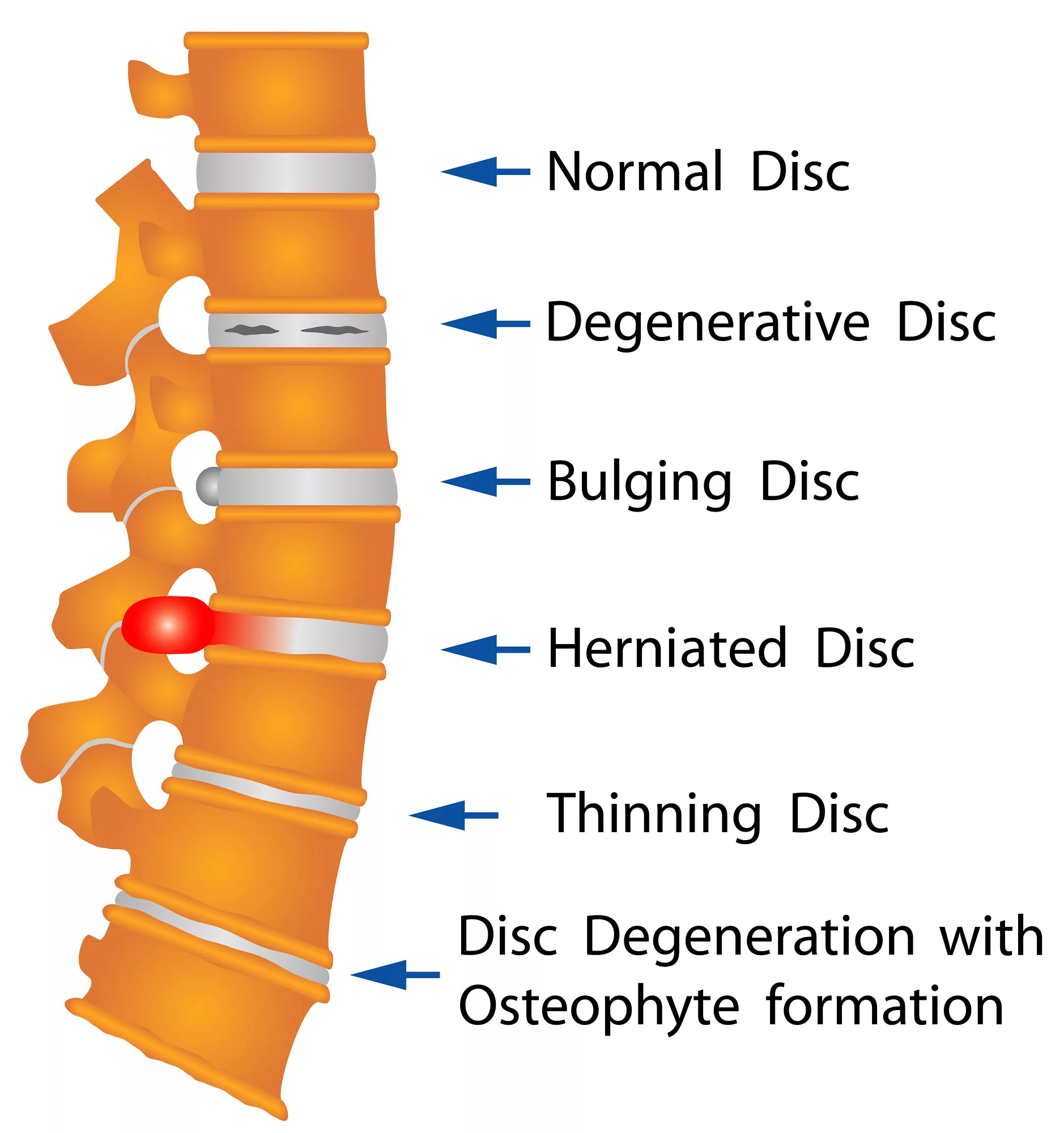
- Age: As we age, the discs in our spine naturally degenerate and become more susceptible to herniation. This is commonly seen in people over the age of 30.
- Trauma or Injury: A sudden force or injury, such as a fall or car accident, can force the nucleus pulposus to rupture through the annulus fibrosus.
- Repetitive Strain: Engaging in activities that involve repetitive bending, twisting, or heavy lifting can put stress on the discs and increase the risk of herniation.
- Genetics: Some individuals may have a genetic predisposition to disc problems, including herniated discs.
- Smoking: Smoking has been linked to disc degeneration, as it can reduce the blood flow to the discs, weakening their structure.
- Obesity: Excess body weight can put additional pressure on the discs, making them more prone to herniation.
- Poor Posture: Maintaining poor posture over time can contribute to disc problems, especially in the neck and lower back.
Signs and Symptoms of a Herniated Disc

Herniated disc can manifest with a wide range of symptoms, and the severity of these symptoms can vary depending on the location of the herniation and the degree of nerve compression. Common signs and symptoms include:
- Pain: This is often the most prominent symptom. The pain can be sharp, shooting, or burning and may radiate along the path of the affected nerve. For example, a herniated disc in the lower back can cause sciatica, which is characterized by pain radiating down the buttock and leg.
- Numbness and Tingling: Herniated discs can lead to numbness and tingling sensations in the affected area. This occurs due to nerve irritation or compression.
- Muscle Weakness: Weakness in specific muscle groups served by the affected nerves may develop. For instance, a herniated disc in the neck can lead to weakness in the arms.
- Loss of Reflexes: Reflexes controlled by the affected nerves may diminish, which can be detected during a physical examination by a healthcare provider.
- Bowel or Bladder Problems: In severe cases, herniated discs in the lower back can compress the cauda equina nerves, leading to loss of bowel or bladder control. This is a medical emergency and requires immediate attention.
It’s important to note that not all herniated disc cause symptoms. Some individuals may have herniated disc that are discovered incidentally during imaging studies conducted for unrelated reasons.
Diagnosing a Herniated Disc

If you suspect you have a herniated disc or are experiencing symptoms, it’s crucial to seek a medical evaluation for an accurate diagnosis. Diagnosing a herniated disc typically involves the following steps:
Medical History and Physical Examination
The process begins with a detailed medical history, during which you’ll discuss your symptoms, medical background, and any recent injuries or activities that may have triggered your symptoms. Following this, a physical examination will be conducted by a healthcare provider to assess your reflexes, muscle strength, and sensation in various areas of your body. They will also look for any signs of nerve irritation.
Imaging Studies
To confirm the diagnosis and visualize the extent of the herniation, healthcare providers may order the following imaging studies:
- Magnetic Resonance Imaging (MRI): This is the most common imaging test for herniated disc. It provides detailed images of the spinal structures and highlights any disc abnormalities, including the location and size of the herniated disc.
- Computed Tomography (CT) Scan: A CT scan may be used to visualize the shape and size of the herniated disc, especially when MRI is contraindicated.
- X-rays: X-rays can help identify any bone spurs or other abnormalities that may be contributing to the problem.
Treatment Options for Herniated Disc

The treatment approach for a herniated disc depends on the severity of your symptoms, the location of the herniation, and your overall health. Treatment options can be broadly categorized into conservative (non-surgical) and surgical approaches.
Conservative Treatment
Conservative treatment methods are typically the first line of defense for herniated disc, and they often include:
- Rest: Taking a break from activities that exacerbate symptoms can allow the body to heal naturally.
- Physical Therapy: A physical therapist can design a customized exercise program to strengthen the surrounding muscles, improve spinal flexibility, and provide techniques to manage pain.
- Medications: Non-steroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants may be prescribed to alleviate pain and inflammation.
- Epidural Steroid Injections: These injections deliver anti-inflammatory medication directly to the affected area to reduce pain and inflammation, providing temporary relief.
- Heat and Ice Therapy: Applying heat or ice to the affected area can help alleviate pain and reduce muscle spasms.
Surgical Treatment
Surgery is considered when conservative treatments fail to provide relief or when severe symptoms, such as muscle weakness or loss of bowel/bladder control, are present. Common surgical procedures for herniated disc include:
- Microdiscectomy: This minimally invasive procedure involves removing the portion of the herniated disc that is pressing on the nerve root. It aims to relieve nerve compression and associated pain.
- Laminectomy: In a laminectomy, a portion of the vertebral bone (lamina) is removed to alleviate pressure on the affected nerve. This procedure is often used for larger herniations or when multiple discs are involved.
- Artificial Disc Replacement: In some cases, the damaged disc may be replaced with an artificial disc to maintain spinal motion and alleviate pain.
- Spinal Fusion: Fusion may be necessary when multiple discs are affected or when there is instability in the spine. It involves fusing two or more vertebrae together using bone grafts and hardware to stabilize the spine.
Rehabilitation
Rehabilitation plays a crucial role in the recovery process following surgery or as part of conservative treatment.It may include:
- Physical Therapy: A tailored program to regain strength, flexibility, and range of motion. Physical therapists can also teach exercises to improve posture and body mechanics.
- Pain Management: Continued use of medications or injections as needed to manage pain and inflammation.
- Education: Learning about proper body mechanics and ergonomics to prevent future disc problems and reduce the risk of re-injury.
- Lifestyle Modifications: Implementing changes in daily activities to reduce strain on the spine, such as lifting techniques and ergonomic workspace adjustments.
Preventing Herniated Disc

While not all herniated disc can be prevented, there are several steps you can take to reduce your risk and promote spine health:
Maintain a Healthy Weight
Excess body weight places added stress on the spine, increasing the risk of herniated disc. Maintaining a healthy weight through a balanced diet and regular exercise can help alleviate this strain.
Practice Good Posture
Proper posture is essential for spine health. When sitting, standing, or lifting objects, maintain a neutral spine position to reduce the risk of disc injuries. Ergonomic adjustments in your workspace can also help maintain good posture.
Exercise Regularly
Strengthening the muscles that support the spine through regular exercise can help prevent herniated disc. Focus on exercises that target the core, back, and abdominal muscles.
Use Proper Lifting Techniques
When lifting heavy objects, bend at the knees and hips while keeping your back straight. Use your leg muscles to lift the load rather than straining the back.
Ergonomics
Ensure that your workspace, whether at home or in the office, is ergonomically designed to reduce strain on the spine. This includes using an adjustable chair, maintaining proper monitor height, and using a keyboard and mouse that promote good wrist posture.
Avoid Smoking
Smoking has been associated with increased disc degeneration. Quitting smoking can help improve spine health and reduce the risk of disc problems.
Stay Hydrated
The discs between your vertebrae need water to maintain their height and function effectively. Staying well-hydrated can help keep your discs healthy and prevent dehydration-related disc issues.
Living with a Herniated Disc

If you’ve been diagnosed with a herniated disc, there are steps you can take to manage your condition and improve your quality of life:
- Follow Your Treatment Plan: Whether you’re undergoing conservative treatment or recovering from surgery, adhere to your healthcare provider’s recommendations. This includes attending physical therapy sessions, taking prescribed medications, and following lifestyle modifications.
- Manage Pain: Learn techniques for managing pain, such as meditation, relaxation exercises, or mindfulness practices. Consult your healthcare provider for pain management strategies tailored to your needs.
- Stay Active: Engage in low-impact activities like swimming or walking to maintain physical fitness and prevent muscle atrophy. Consult with your healthcare provider or physical therapist to determine appropriate exercises for your condition.
- Supportive Devices: Consider using supportive devices such as lumbar cushions, braces, or ergonomic furniture to reduce discomfort during daily activities and promote proper spinal alignment.
- Stay Informed: Educate yourself about your condition and available treatment options. Being informed empowers you to make decisions about your health and participate actively in your treatment plan.
- Seek Support: Coping with a herniated disc can be emotionally challenging. Consider joining support groups or seeking counseling to receive emotional support and practical advice during your recovery journey.
Conclusion: Herniated Disc

In conclusion, a herniated disc can be a painful and life-disrupting condition, but with the right knowledge, early intervention, and a commitment to preventive measures, you can effectively manage this condition and minimize its impact on your daily life. Remember that seeking medical evaluation and following a tailored treatment plan are essential steps towards recovery. Whether you’re focused on preventing herniated disc or navigating life with an existing diagnosis, prioritize spine health through proper posture, regular exercise, and lifestyle modifications. By taking proactive steps and working closely with healthcare professionals, you can promote a healthier, more active life and reduce the risk of herniated discs in the long run.
BEST CHIROPRACTOR NEAR ME IN ORLANDO, FLORIDA
CALL NOW +1-407-434-7246
If you have suffered any type of injury or have been experiencing pain that just won’t go away regardless of what you do, then all you have to do is call and speak with our friendly staff. Find Best Sciatica Chiropractor in Orlando, Florida. Our team can help you get the treatment you need and ensure that the pain you experience is alleviated – once and for all.
We are proud to serve the areas of Orlando, Altamonte Springs, Haines City, Plant City, Kissimmee, Winter Haven, and Ocala.
Contact us for Chiropractor near me in Orlando, Florida for an Appointment Today.
Can a herniated disc heal itself?
Herniated disks get better on their own over time or with nonsurgical treatment for 9 out of 10 people. If other treatments don't relieve your symptoms, your healthcare provider may recommend surgery.
What is the main cause of a herniated disc?
The most common cause of disc herniation is a degenerative process in which, as humans age, the nucleus pulposus becomes less hydrated and weakens. This process will lead to a progressive disc herniation that can cause symptoms. The second most common cause of disc herniation is trauma.
Is walking good for herniated disc?
Low-impact exercises, such as walking, swimming, and cycling, may be safe and beneficial for people with a herniated disc, as they can help to improve overall fitness and strengthen the muscles that support the spine.
Is a herniated disc life long?
Harvard Health reports approximately 90 percent of the time, herniated disc symptoms go away within six months with little or no significant intervention. This can happen even if the damage to the affected disc is technically still present and detectable on image tests.
How do you sleep with a herniated disc?
Sleeping on your back is one of the best positions to sleep for herniated discs. It allows your weight to be evenly distributed and spread across your body. As a result, you can put less strain on your pressure points.