Understanding Fibromyalgia: Unraveling the Mystery of Chronic Pain
Fibromyalgia is a complex and often misunderstood medical condition that affects millions of people worldwide. Despite its prevalence, it remains a condition shrouded in mystery, both for those who suffer from it and for many in the medical community. Fibromyalgia is a chronic medical condition characterized by widespread musculoskeletal pain, fatigue, and tender points. It is considered a complex and often poorly understood disorder, leading to challenges in diagnosis and treatment. In this blog post, we will explore what is fibromyalgia, its symptoms, causes, diagnosis, treatment options, and tips for managing this challenging condition.
What is Fibromyalgia?

Fibromyalgia, often referred to as FM, is a chronic pain disorder characterized by widespread musculoskeletal pain, fatigue, and tender points throughout the body. The pain experienced by fibromyalgia patients is often described as a constant dull ache that can last for months or even years. It is a long-term, debilitating condition that affects people of all ages, genders, and backgrounds.
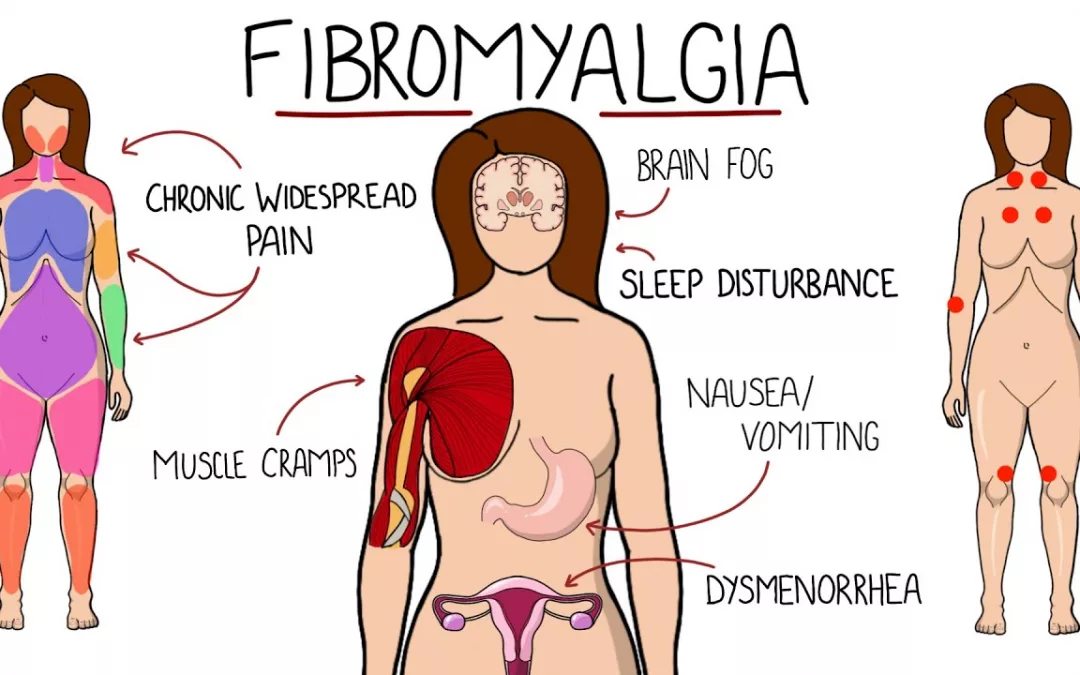
Symptoms of Fibromyalgia

Fibromyalgia is a complex and chronic condition with a wide range of symptoms. These symptoms can vary in intensity and may come and go. The most common symptoms of fibromyalgia include:
Widespread Pain: The primary symptom of fibromyalgia is widespread, chronic pain. This pain is often described as a deep, persistent ache that affects both sides of the body. It typically occurs in specific areas, such as the neck, shoulders, back, hips, and limbs. The pain can migrate or change in intensity and is often accompanied by tenderness at specific points on the body.
- Fatigue: Individuals with fibromyalgia often experience significant fatigue, even after a full night’s sleep. This fatigue can be debilitating and may interfere with daily activities and work.
- Tender Points: There are 18 designated tender points on the body that are associated with fibromyalgia. These points are typically located at the back of the neck, the shoulders, the chest, the lower back, the hips, the elbows, and the knees. Applying pressure to these points can cause significant pain and discomfort.
- Sleep Disturbances: Many people with fibromyalgia suffer from sleep disturbances. These can include difficulties falling asleep, staying asleep, and achieving restorative sleep. Poor sleep quality can exacerbate other symptoms.
- Cognitive Issues: Fibromyalgia is often linked to cognitive issues commonly referred to as “fibro fog.” This can involve memory problems, difficulty concentrating, mental confusion, and impaired cognitive function.
- Headaches: Frequent tension headaches and migraines are common in individuals with fibromyalgia.
- Sensitivity to Stimuli: People with fibromyalgia often have heightened sensitivity to sensory stimuli, such as light, noise, temperature changes, and even certain odors. This heightened sensitivity can exacerbate discomfort.
- Irritable Bowel Syndrome (IBS): Many individuals with fibromyalgia also experience symptoms of IBS, including abdominal pain, diarrhea, constipation, and other gastrointestinal issues.
- Depression and Anxiety: Living with chronic pain and fatigue can lead to emotional challenges, including depression and anxiety. These mental health issues often coexist with fibromyalgia.
It’s important to note that fibromyalgia symptoms can vary from person to person, and not everyone with the condition will experience all of these symptoms. Additionally, these symptoms can come and go, and their severity can change over time. Fibromyalgia can be challenging to diagnose and manage because of the complexity of its symptoms and the lack of definitive diagnostic tests. Therefore, a comprehensive evaluation by a healthcare provider with experience in treating fibromyalgia is essential to establish an accurate diagnosis and develop a tailored treatment plan.
Causes of Fibromyalgia

The exact causes of fibromyalgia are not fully understood, and it’s likely that multiple factors contribute to the development of this complex condition. Researchers have proposed several potential causes and triggers, but no single cause has been definitively identified. Here are some of the factors that are believed to play a role in the development of fibromyalgia:
- Genetics: Genetic factors may predispose some individuals to fibromyalgia. There is evidence that the condition can run in families, suggesting a hereditary component. Certain genetic variations may influence an individual’s susceptibility to developing fibromyalgia.
- Abnormal Pain Processing: Fibromyalgia is often associated with abnormalities in how the central nervous system processes pain signals. People with fibromyalgia may have an increased sensitivity to pain and a lower threshold for pain. This altered pain processing can lead to the widespread pain and tenderness characteristic of the condition.
- Infections: In some cases, infections, particularly viral infections, have been identified as potential triggers for fibromyalgia. It’s thought that an infection may activate or exacerbate the condition in some individuals.
- Physical or Emotional Trauma: Physical trauma, such as car accidents, injuries, or surgery, can be a triggering event for fibromyalgia symptoms. Emotional trauma, such as post-traumatic stress disorder (PTSD), can also play a role. Trauma can lead to changes in the way the central nervous system processes pain signals.
- Hormonal Changes: Hormonal fluctuations, such as those occurring during menopause, pregnancy, or the menstrual cycle, may influence the onset or exacerbation of fibromyalgia symptoms. Some women experience their first symptoms of fibromyalgia during these hormonal changes.
- Autoimmune Disorders: Some researchers have explored the possibility of autoimmune factors contributing to fibromyalgia. While not an autoimmune disease in the traditional sense, there may be immune system dysregulation in some individuals with fibromyalgia.
- Other Chronic Conditions: Fibromyalgia is known to commonly coexist with other chronic conditions such as rheumatoid arthritis, lupus, and irritable bowel syndrome (IBS). It is unclear whether fibromyalgia is a result of these conditions or if they share common underlying factors.
- Psychological Factors: While not a direct cause of fibromyalgia, psychological factors such as stress, anxiety, and depression can exacerbate the symptoms and decrease an individual’s tolerance for pain. These factors may also influence the perception of pain in those with fibromyalgia.
It’s important to note that the exact interplay between these factors and the development of fibromyalgia remains a subject of ongoing research and debate. As a result, there is no single test or diagnostic marker for fibromyalgia, and its diagnosis typically relies on clinical evaluation and the presence of specific symptoms.
Additionally, fibromyalgia is a highly individualized condition, and what triggers or exacerbates symptoms in one person may not do the same for another. Treatment for fibromyalgia often involves a multidisciplinary approach to manage the symptoms and improve an individual’s quality of life, and it may include medication, physical therapy, lifestyle modifications, and psychological support.
Fibromyalgia Diagnosis

Diagnosing fibromyalgia can be challenging because there are no specific tests or imaging studies that can definitively confirm its presence. Instead, healthcare providers rely on a combination of clinical criteria and a patient’s medical history to make a diagnosis. Here’s a detailed explanation of the diagnostic process for fibromyalgia:
- Medical History: The first step in diagnosing fibromyalgia is a thorough medical history. Your healthcare provider will ask about your symptoms, their duration, and their impact on your daily life. It’s important to provide detailed information about the location, type, and intensity of your pain and any other symptoms you may be experiencing.
- Physical Examination: During the physical examination, your healthcare provider will check for the presence of specific tender points on your body. There are 18 designated tender points used for diagnosing fibromyalgia. These points are typically located in pairs on the back of the neck, shoulders, chest, lower back, hips, elbows, and knees. Your healthcare provider will apply pressure to these points to assess your pain response.
- Exclusion of Other Conditions: Part of the diagnostic process involves ruling out other medical conditions that can mimic the symptoms of fibromyalgia. Conditions like rheumatoid arthritis, lupus, and thyroid disorders can have similar symptoms, and specific tests may be performed to eliminate these as potential causes of your pain and discomfort.
- American College of Rheumatology (ACR) Criteria: Historically, the American College of Rheumatology (ACR) criteria have been widely used for diagnosing fibromyalgia. These criteria require the presence of widespread pain lasting for at least three months and the identification of tender points. According to the ACR, a person must have at least 11 of the 18 specified tender points to meet the criteria.
- 2016 ACR Criteria: In 2016, the ACR introduced updated criteria for fibromyalgia diagnosis. These criteria are more inclusive and consider other symptoms besides pain and tender points. They take into account the severity of pain, fatigue, sleep problems, and cognitive symptoms. The diagnosis is based on a scoring system that evaluates the extent and intensity of symptoms.
- Patient Questionnaires: Healthcare providers may use patient questionnaires to assess the presence and impact of various symptoms. These questionnaires may cover pain, fatigue, sleep quality, cognitive function, and psychological well-being.
It’s important to note that the diagnosis of fibromyalgia is primarily a clinical one, and the process may vary depending on the healthcare provider’s approach. In some cases, a rheumatologist or a specialist in pain management may be involved in the diagnosis and management of fibromyalgia.
Given the complex nature of fibromyalgia and the absence of specific diagnostic tests, obtaining an accurate diagnosis often requires patience and cooperation between the patient and the healthcare provider. Once a diagnosis is established, the focus shifts to developing a treatment plan tailored to the individual’s specific symptoms and needs. This plan may include a combination of medication, physical therapy, lifestyle modifications, and psychological support to help manage the condition and improve the patient’s quality of life.
Fibromyalgia Treatment Options

Fibromyalgia is a chronic condition with no known cure, but there are various treatment options available to help manage its symptoms and improve the quality of life for individuals affected by it. The treatment plan for fibromyalgia is often individualized, as it depends on the specific symptoms and needs of each patient. Here are common treatment approaches for fibromyalgia:
- Medications:
- Pain Relievers: Over-the-counter pain relievers such as ibuprofen or acetaminophen may provide some relief from pain. Prescription medications, such as tramadol, may be considered for more severe pain.
- Antidepressants: Certain classes of antidepressant medications are often used to manage fibromyalgia symptoms. These include:
- Duloxetine (Cymbalta): This medication can help reduce pain and improve mood.
- Amitriptyline (Elavil): It may be prescribed at lower doses than typically used for depression to improve sleep and alleviate pain.
- Antiseizure Drugs: Medications like gabapentin (Neurontin) and pregabalin (Lyrica) can help reduce pain and improve sleep quality.
- Physical Therapy: Physical therapists can work with individuals with fibromyalgia to improve flexibility, strength, and mobility. Exercises and techniques designed for fibromyalgia patients aim to alleviate pain and stiffness. Aquatic therapy is often recommended because it is gentle on the joints.
- Occupational Therapy: Occupational therapists can provide strategies to make daily activities and tasks more manageable for individuals with fibromyalgia. This may include recommendations for ergonomic modifications and adaptive tools.
- Counseling and Cognitive-Behavioral Therapy (CBT): CBT is a type of psychotherapy that helps individuals with fibromyalgia manage the emotional and psychological aspects of living with chronic pain. It can teach coping strategies, relaxation techniques, and ways to improve sleep.
- Lifestyle Modifications:
- Exercise: Engaging in regular, low-impact exercise can help reduce pain and improve overall well-being. Activities like swimming, walking, yoga, and tai chi are often recommended. Exercise should be gradual and tailored to individual capabilities to avoid exacerbating symptoms.
- Stress Management: Stress reduction techniques, such as meditation, deep breathing exercises, and mindfulness, can help individuals manage the emotional aspects of fibromyalgia.
- Sleep Hygiene: Creating a comfortable sleep environment and practicing good sleep habits can improve sleep quality.
- Dietary Changes: Some individuals with fibromyalgia find symptom relief by making dietary modifications. This may include avoiding certain trigger foods or incorporating anti-inflammatory foods into their diet.
- Complementary and Alternative Therapies: Some individuals explore alternative treatments, such as acupuncture, massage therapy, chiropractic care, and myofascial release therapy. While the evidence for their effectiveness is mixed, some patients report benefits from these therapies.
- Support Groups: Joining a fibromyalgia support group can be beneficial for individuals seeking emotional support and advice from others who understand their condition. Sharing experiences and coping strategies can be invaluable.
- Medication Management: It is essential to regularly review and adjust medications with a healthcare provider to ensure optimal symptom management. Medication management is especially important for individuals taking antidepressants, antiseizure drugs, or pain relievers.
- Alternative Treatments: Some individuals explore complementary and alternative treatments, such as medical cannabis, to alleviate their symptoms. It’s important to consult with a healthcare provider before considering such options.
Fibromyalgia treatment often involves a multidisciplinary approach, with healthcare providers collaborating to develop a comprehensive treatment plan tailored to the individual’s specific needs. While there is no one-size-fits-all solution, many people with fibromyalgia find relief and improved quality of life through a combination of these treatment approaches. It’s essential for individuals to work closely with their healthcare team to manage their condition effectively.
Living with Fibromyalgia

Living with fibromyalgia can be challenging, as the condition often presents a range of physical and emotional symptoms that can significantly impact your quality of life. However, with the right strategies and support, many individuals with fibromyalgia can manage their symptoms and improve their well-being. Here are some tips for living with fibromyalgia:
- Pace Yourself: One of the most important principles for managing fibromyalgia is learning to pace yourself. Avoid overexertion and set realistic limits on your activities. Prioritize tasks and take breaks when needed to prevent symptom flare-ups.
- Get Quality Sleep: Establish a consistent sleep routine and create a comfortable sleeping environment. Good sleep hygiene practices can help improve the quality of your sleep, which is essential for managing fibromyalgia symptoms.
- Exercise Regularly: Engaging in regular, low-impact exercise can help improve flexibility, strength, and reduce pain. Consult with a physical therapist or a healthcare provider to develop a personalized exercise plan that suits your abilities and needs.
- Stress Management: Practice stress-reduction techniques, such as meditation, deep breathing exercises, progressive muscle relaxation, or mindfulness. Managing stress can help reduce the impact of emotional symptoms and improve overall well-being.
- Dietary Considerations: Pay attention to your diet. Some individuals with fibromyalgia find symptom relief by making dietary changes. This may involve avoiding certain trigger foods or incorporating anti-inflammatory foods into your meals.
- Stay Informed: Knowledge is empowering. Stay informed about fibromyalgia by seeking reliable sources of information. Understanding your condition and the available treatment options can help you make informed decisions about your health.
- Support Network: Connect with others who have fibromyalgia through support groups, either in person or online. Sharing experiences and advice can be invaluable for coping with the challenges of living with fibromyalgia.
- Communication with Your Healthcare Team: Maintain open and regular communication with your healthcare provider. Discuss your symptoms, treatment plan, and any concerns or questions you may have. Your healthcare team can help you adjust your treatment plan as needed.
- Manage Your Emotions: Living with fibromyalgia can be emotionally challenging. It’s important to acknowledge and address the emotional impact of the condition. Consider seeking support from a mental health professional or counselor to manage anxiety, depression, and stress.
- Adaptive Tools and Techniques: Consider using adaptive tools and techniques to make daily activities more manageable. Occupational therapists can provide guidance on how to modify your environment and routines to accommodate your condition.
- Prioritize Self-Care: Prioritize self-care activities that help you relax and rejuvenate. Whether it’s reading, taking a warm bath, practicing hobbies, or spending time with loved ones, self-care is essential for overall well-being.
- Seek Consistent Treatment: Continue with consistent treatment, including medications and therapies, as recommended by your healthcare provider. Regular check-ins will help ensure that your treatment plan is effective and can be adjusted as needed.
Remember that living with fibromyalgia may have ups and downs, and the severity of symptoms can vary. It’s important to be patient with yourself and make self-care a priority. While there may be no cure for fibromyalgia, many individuals can successfully manage their symptoms and lead fulfilling lives by implementing these strategies and seeking the support they need.
Conclusion: What is Fibromyalgia?

Fibromyalgia is a chronic pain condition that affects millions of people around the world. While it remains a complex and enigmatic condition, advances in research and medical understanding are continually improving the management of its symptoms. Living with fibromyalgia can be challenging, but with the right support and a comprehensive treatment plan, individuals can lead fulfilling lives and reduce the impact of this condition on their overall well-being. If you or someone you know is struggling with fibromyalgia, remember that seeking professional medical guidance and emotional support is key to effectively managing the condition. With continued research and a supportive healthcare community, the future holds promise for better management and, hopefully, one day, a cure for fibromyalgia.
BEST CHIROPRACTOR NEAR ME IN ORLANDO, FLORIDA
CALL NOW +1-407-434-7246
If you have suffered any type of injury or have been experiencing pain that just won’t go away regardless of what you do, then all you have to do is call and speak with our friendly staff. Find Best Chiropractic Care in Orlando, Florida. Our team can help you get the treatment you need and ensure that the pain you experience is alleviated – once and for all.
We are proud to serve the areas of Orlando, Altamonte Springs, Haines City, Plant City, Kissimmee, Winter Haven, and Ocala.
Contact us for Chiropractor near me in Orlando, Florida for an Appointment Today.
What is fibromyalgia caused by?
Stressful or traumatic events, such as car accidents, post-traumatic stress disorder (PTSD) Repetitive injuries. Injury from repetitive stress on a joint, such as frequent knee bending. Illness (such as viral infections).
What are the five symptoms of fibromyalgia?
Fibromyalgia is a condition in which a person has long-term pain that is spread throughout the body. The pain is most often accompanied by fatigue, sleep problems, difficulty concentrating, headaches, depression, and anxiety.
Does fibromyalgia ever go away?
There's no cure for fibromyalgia, but the condition may go into remission for weeks or even years at a time. Even though fibromyalgia is considered a chronic condition that never goes away entirely, most people experience fluctuations in symptoms over time.
How do you confirm fibromyalgia?
Fibromyalgia is diagnosed based primarily on having pain all over the body, along with other symptoms. Currently, there are no specific laboratory or imaging tests for fibromyalgia.
What organ does fibromyalgia affect?
Fibromyalgia was formerly classified as an inflammatory musculoskeletal disease but is now considered to be an illness that primarily affects the central nervous system.